Past Issues
Marchiafava-Bignami: Clinical Case Description
Milton CR Medeiros1,*, Milton Takeshi Medeiros2, Marilia Mancebo3
1Irmandade Santa Casa de Arapongas, Rua Calu, 155, Arapongas PR, Brazil
2,3Centro Universitário de Valença – UNIFAA, Rua sargento Vitor Hugo, 161, Valença RJ, Brazil
*Corresponding author: Milton CR Medeiros, Irmandade Santa Casa de Arapongas, Rua Calu, 155, Arapongas PR, Brazil, Tel: 43999728197, E-mail: [email protected]
Received Date: August 19, 2024
Publication Date: August 29, 2024
Citation: Medeiros MCR, et al. (2024). Marchiafava-Bignami: Clinical Case Description. Neuro Research. 6(1):19.
Copyright: Medeiros MCR, et al. © (2024).
ABSTRACT
Introdution: Marchiafava-Bignami disease is a rare disorder of demyelination and necrosis of the corpus callosum and the near subcortical white matter that is especially predominant in chronic alcoholism. It was discovered in 1903 by Italian pathologists Ettore Marchiafava and Amico Bignami. They described a case that presented necrosis of their corpus callosum on autopsy. Just a few cases have been described in non-drinking patients, suggesting that alcohol is the main, but not the only responsible for these disease. Its development is also possible in chronic malnutrition. The main pathophysiological hypothesis is the deficiency of B complex vitamins. Replacement of B complex vitamins guides the current treatment, although there is not always a significant improvement in the clinical picture, as happened in the case described. Case Presentation: male patient, 68 years old. Chronic alcoholic with daily consumption of distilled drinks. Since two years ago he had been experiencing progressive cognitive decline across multiple domains. On physical examination, he presented mini mental status exam 18 (spatial disorientation, recall memory and language), gait disturbance and bilateral pyramidal signs. He received intravenous hydration, calories and B-complex vitamins, with only slight improvement after 7 days of hospitalization. MRI showed hyperintense signal on T2 affecting the corpus callosum. After one month of outpatient follow-up, the patient showed a slight improvement in gait, but maintained cognitive impairment. Discussion: Marchiafa-Bignami disease should be remembered in chronic alcoholics with non-specific neurodegenerative symptoms. History, physical examination and MRI can lead to the diagnosis, guiding treatment. Final Comments: chronic alcoholic patients with a non-specific neurodegenerative condition must have Marchiafava-Bignami disease on the list of differential diagnoses. History, physical examination and magnetic resonance imaging define the diagnosis, allowing prompt treatment. Unfortunately, in the case described, even with appropriate therapeutic measures, there was no good evolution. Probably due to the significant extent of the lesion in the corpus callosum.
Keywords: Marchiafava-Bignami, Chronic Alcoholism, Corpus Callosum, Complex B Vitamin
INTRODUTION
Marchiafava-Bignami disease is a very rare disorder characterized by demyelination and necrosis of the corpus callosum. Some times adjacent subcortical white matter may also be involved. The disease was first described in 1903 by Italian pathologists Ettore Marchiafava and Amico Bignami [1]. They described a man with alcohol use disorder who died of neurodegenerative condition, with refractory epileptic seizures and coma. At autopsy, the patient presented necrosis of the corpus callosum. The main pathologic changes seen in Marchiafava-Bignami include symmetrical demyelination and necrosis of the central part of the corpus callosum. Other structures of the central nervous system like putamen, optic chiasm and tracts, anterior commissure, cerebellar peduncles and cortical gray matter and U fibers may be involved [2]. The pathophysiology is unclear, but we know that Ethanol is an important risk factor for various brain disorders, depending on the amount and frequency of its use. The association of alcohol with B-complex hypovitaminosis, especially thiamine, can directly damage the corpus callosum, producing an initial phase of cytotoxic edema and breakdown of the blood-brain barrier. The consequences are demyelination, necrosis and subsequent atrophy. The neuroradiological classification of Marchiafava-Bignami shows two subtypes of the disease [3]. Type A, characterized by acute or subacute onset of consciousness impairment, pyramidal tract signs, limb hypertonia and seizures. In these cases there is extensive involvement of the corpus callosum. On magnetic ressonance imaging (MRI), hyperintense signal on T2 and FLAIR is observed in a large part of the corpus callosum. This type is associated with poor prognosis. In type B, there is preservation of the level of consciousness, with gait disturbance and signs of interhemispheric disconnection. In this type, the prognosis is better than in type A. Type B radiological findings are T2-weighted MR sequences partially involving the corpus callosum. There is a Variable clinical spectrum, defined by characteristics lesions in the corpus callosum. Early symptoms are typically mental, including mania, depression, paranoia and dementia. Sometimes the disease presents itself only as psychiatic signs and symptoms [4]. These patients are often malnourished and have water and electrolyte disorders. Treatment basically consists of replacing calories, good fluid and electrolyte replacement and supplementation of B complex vitamins, especially thiamine. Thiamine can be used in the folowing dose: 200 to 500 mg intravenously three times a day for 2 to 7 days. Lastly, an oral maintenance dose of 100 mg once each day [5]. Megaloblastic and macrocytic anemias linked to alcohol use disorder and malnutrition can be treated or prevented by supplementing with folic acid at 1 to 5 mg taken orally once daily. Research shows that steroid use is not effective [6].
CASE PRESENTATION
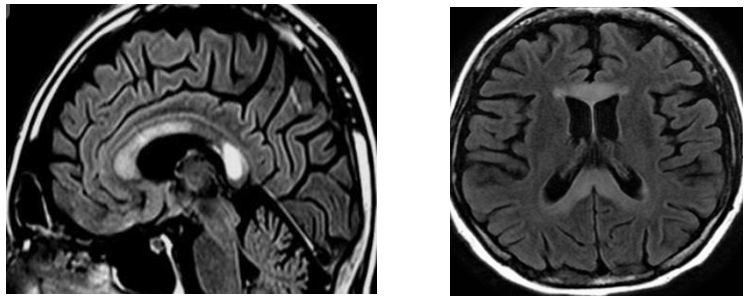
We followed a 68 years old patient, chronic alcoholic, who had consumed distilled drinks daily for over 25 years. The patient had progressive cognitive decline for 1 year, with involvement of more than one cognitive domain. The result of the mini mental state exam was 18 (literate patient, but without a university degree). He presented spatial disorientation, working memory difficulty, language disorder and difficulty concentrating. He presented gait disturbance and signs of bilateral pyramidal involvement. No depression of the level of consciousness was observed. The cranial nerves were preserved on physical examination, an important finding for the differentiation of wernicke-Korsakoff syndrome. Laboratorial tests showed only mild hyponatremia. MRI showed hyperintense signal on T2 and FLAIR affecting the corpus callosum (Figure 1). He received intravenous hydration, calories and B complex vitamins, with an emphasis on vitamin B1.
RESULTS
The patient showed a small improvement after 7 days of hospitalization, being discharged from the hospital and scheduled to return to the outpatient clinic, using B vitamis and caloric supplementation. After 1 month, on outpatient follow-up, the patient showed some improvement in gait, but maintained cognitive changes. The most important deficiences were in working memory and concentration, disabling the patient in decision making.
Figure 1. MRI showed hyperintense signal on FLAIR affecting the corpus callosum.
DISCUSSION
Marchiafa-Bignami disease should be remembered in chronic alcoholics with non-specific neurodegenerative symptoms. History, physical examination and MRI can lead to the diagnosis, guiding treatment. The treatment should be started as soon as possible with nutritional support, hydration and supplementation of B vitamins, especially thiamine. In some cases, there may be complete recovery of the condition, as in the case description by Vineet and collaborators [7], where there was recovery from a condition with a predominance of dementia.
FINAL COMMENTS
The disease severity is variable, as like the prognosis. It is hypothesized that incomplete lesions with sparing of the superior commissure fibers are associated with better prognosis. Early diagnosis and effective treatment are important to the patient’s recovery. Unfortunately, in the case described, even with appropriate therapeutic measures, there was no good evolution, probably due to the significant extent of the lesion in the corpus callosum.
CONCLUSION
In conclusion, chronic alcoholic patients with a non-specific neurodegenerative condition must have Marchiafava-Bignami disease on the list of differential diagnoses. History, physical examination and magnetic resonance imaging define the diagnosis, allowing prompt treatment.
REFERENCES
- Tian TY, Ruschel MAP, Park S, Liang. JW. (2023). Marchiafava-Bignami. Treasure Island (FL): StatPearls Publishing.
- Gambini A, Falini A, Moiola L, Comi G, Scotti G. (2003). Marchiafava-Bignami Disease: Longitudinal MR Imaging and MR Spectroscopy Study. Am J Neuroradiol. 24(2):249-253.
- Kumar K S, Challam R, J N, Singh WJ. (2014). Marchiafava - bignami disease: a case report. J Clin Diagn Res. 8(8):RD01- RD02.
- Sönmes D, Hocaoglu C. (2023). Marchiafava-Bignami disease presenting with psychiatric symptoms: A case report. Psychiatry Research Case Reports. 2(2):100174.
- Sechi G, Serra A. (2007). Wernicke's encephalopathy: new clinical settings and recent advances in diagnosis and management. Lancet Neurol. 6(5):442-455.
- Hillbom M, Saloheimo P, Fujioka S, Wszolek ZK, Juvela S, Leone MA. (2014). Diagnosis and management of Marchiafava-Bignami disease: a review of CT - MRI confirmed cases. J Neurol Neurosurg Psychiatry. 85(2):168-173.
- Sehgal V, Kesav P, Modi M, Ahuja CK. (2013). Acute Marchiafava-Bignami disease presenting as reversible dementia in a chronic alcoholic. BMJ Case Rep. 2013:bcr2012008286.
 Abstract
Abstract  PDF
PDF